Insurance claims are a critical part of the customer experience, in fact, the time taken for an insurance company to satisfactorily settle a claim is viewed as the number one measure of customer satisfaction. After paying premiums for years together, claims are the first and only direct interaction between the client and the insurance provider. They expect immediate attention and care, and a poor customer experience can create enough dissatisfaction that the client seeks a different insurance provider.
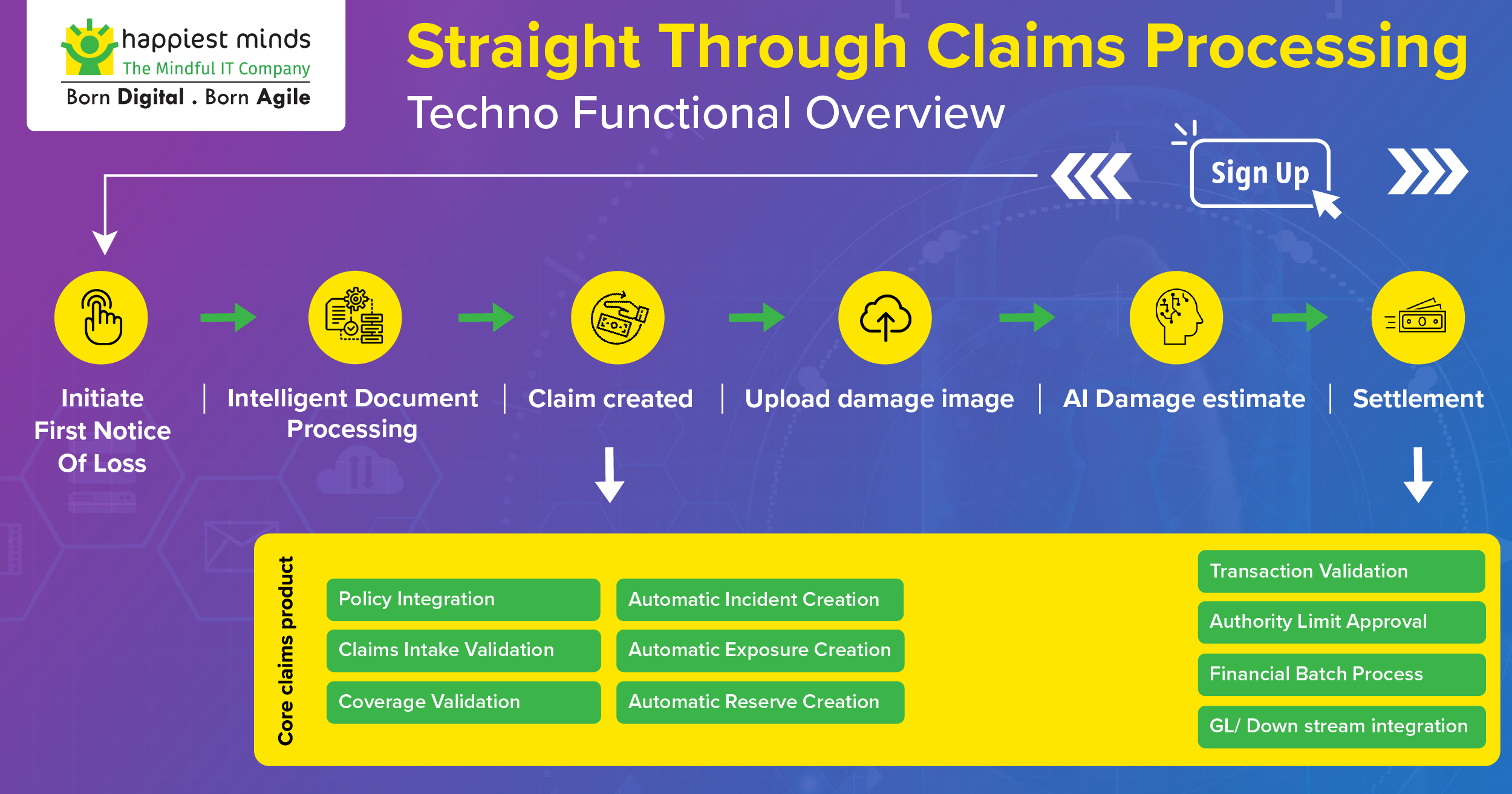
We are in 2023, and most insurance companies have moved from a legacy claims platform to a modern claims management platform. Especially in the property and casualty industry, most modern claim management systems come with an enhanced and efficient business process for claim intake, adjudication, and settlement. Most of these business processes are driven by static & dynamic rules and often lacks intelligence. Straight Through Processing is a term coined for an FNOL request that passes through a set of business processes, straight through to the settlement. But compared to the InsurTech startups which have Artificial intelligence, machine learning, and Intelligent process automation as the core, the modern claim management systems still have a lot of scope for improvement.
Key areas of improvement for Next-gen Straight-through Processing system
- Digital Portals – Transition from process-centric to customer-centric intake
The core insurance products were designed and built primarily to cater to internal insurance employees. This includes the adjusters, claim handlers, CSRs, and supervisors. Its core objective was to enhance the insurance business process backed by modern software platforms moving away from legacy systems. Now, more than ever there is a need to expose part of these services to the end customers, and hence the need for self-servicing applications has exponentially increased. The core product is already well integrated with fraud, financial reporting, and downstream systems with ample customizations and care should be taken to leverage them as well. “The front-end portals should embrace and co-exist with the core insurance product to deliver maximum functional and cost value.”
- Self-servicing capabilities not just for one, but for most lines of businesses
While implementing an external portal, longer time to market, ease of enhancement, and maintenance cost remain other major problems. Because of these reasons most carriers start with self-servicing portals for one line of business (mostly personal auto) but wouldn’t implement them for the rest of their product offerings. A lot of thought should be put in while deciding on the front-end platform for digital portal implementation. “Lately low code platforms like Appian, Outsystems, and ServiceNow offers plethora of features with an aim to reduce the implementation and maintenance cost permanently.”
- An efficient System of Engagement
One of the key features of portals is the First Notice of Loss (FNOL) or the claims intake process. In a B2C scenario, a system of engagement is a must to intake critical information from the end customer, while incorporating varying degrees of video, photos, and voice-to-text features. Also, in a B2B scenario, the agents should have the capability to consolidate the incoming claim requests and information updates from multiple channels to continue the settlement process seamlessly. An Open API-backed platform is preferred because it integrates with a wide range of external systems. “Overall, an efficient system of engagement can integrate with multiple external systems of records and present a unified view which is proven to accelerate business process Ex: complaints consolidation, 360 customer view, Invoice processing, vendor service requests.”
- Look beyond rule-based automation. Embrace AI/ML/RPA
Automating parts of the claims journey reduces manual work and improves claim settlement accuracy. RPA when combined with advanced analytics or Machine Learning (ML) models can help interpret texts, process processing intake documents, and invoices, engage in chat conversations, and even drive autonomous decision-making. With the help of special AI-based algorithms and vision analytics models, the loss damage assessment and loss appraisal can be done in minutes-hours as compared to the traditional way of assessment which takes days-weeks-months.
Currently, there isn’t a one-stop shop for all the insurance process automation /analytics available, and usually, insurance carriers consider external third-party vendors for a quicker turnaround time. At the same time, involving multiple third-party vendors increases the risk of data security and data being monetized without the carrier’s consent.
- Transition from repair-replace to predict-prevent risk management philosophy
Touchless claims or even better, preventing a loss from occurring are going to be the evolution of the straight through processing systems. More data has been created in the last couple of years than in the entire history of humans. Thanks to the wider adoption of IoT and connected devices which facilitates forming data lakes. Analytics applied to these large datasets help carriers to generate actionable insight and support decision-making.
Out of the four broader categories of data analytics, namely 1. Descriptive Analytics 2. Diagnostic Analytics 3. Predictive Analytics 4. Prescriptive Analytics, #3 and 4# are of primary focus in the insurance industry.
Sensors in buildings can alert owners and insurers when temperatures breach the threshold to freeze pipes and automatically trigger integrated smart thermostats to turn up the heat. Similarly, in the manual labor workplace, sensors embedded in workers’ clothing and telematics sensors can monitor movements, and if there is a breach of the safe zone, machines can be stopped automatically, preventing injury.
Happiest Minds Solution: “Nexurance – A Next-gen Straight-through processing system”
What if the key improvements mentioned above are already available as a solution and come integrated with a core insurance product? Our Nexurance straight through processing system leverages the Low-Code front-end portals, IDP, and Vision analytics model to provide a seamless claim processing experience.
Write to [email protected] to learn more about our Nexurance solution offerings or for a Demo.

is a Guidewire certified Ace and the Senior Architect, for Digital Business Services at Happiest Minds. He has an overall experience of 13+ years in the BFSI industry. He specializes in large-scale business transformation of Insurance applications, involving full suite implementation and Major upgrades across APAC, Americas & Europe.